Project Introduction
Quantification of the left ventricle (LV) shape is critical in evaluating cardiac function from 2D echocardiographic images.
This study investigates the impact of different loss functions on the optimisation of the U-Net model for LV segmentation.
Our results reveal that the choice of loss function plays a significant role in achieving accurate LV volume measurements — even when traditional segmentation metrics like Dice coefficient show minimal change.
Dataset
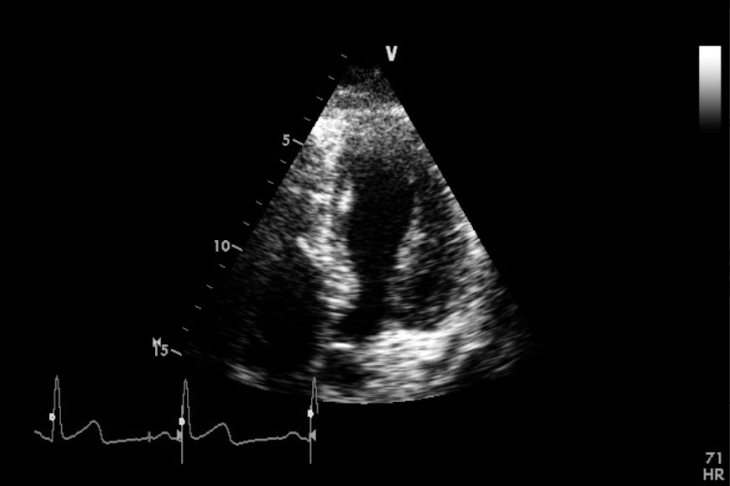
Fig. 1. Example from the dataset.
A total of 1,224 apical 4-chamber echocardiographic videos (2015–2016) were collected from Imperial College Healthcare NHS Trust’s database.
Images were acquired using GE and Philips ultrasound systems by experienced echocardiographers following standard protocols.
- Ethics: Approved by the Health Regulatory Agency (IRAS ID: 243023)
- Development dataset: 2,600 images, annotated by experts using the Unity Imaging Platform
- Testing dataset: 100 videos from 2019, with 200 frames (end-diastolic & end-systolic)
- Each image was annotated by 11 human experts, and the consensus annotation was used as ground truth.
Method
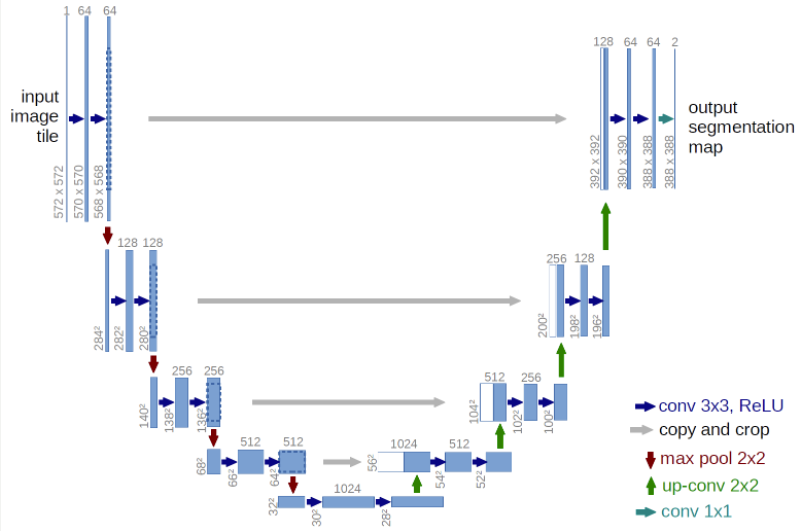
Fig. 2. U-Net architecture used in this study.
The U-Net model was implemented in TensorFlow and trained on an NVIDIA RTX3090 GPU.
The following loss functions were evaluated, covering three categories:
- Distribution-based: Binary Cross Entropy (BCE)
- Region-based: Dice, Tversky, Focal Tversky
- Compound: BCE + Dice
After training, model performance was evaluated using both segmentation metrics and domain-specific cardiac metrics:
- Dice Coefficient (DC) and Hausdorff Distance (HD) for segmentation
- Volume Error and Ejection Fraction (EF) for clinical relevance
Volumes were computed using Simpson’s method, and EF was calculated as:
[ EF = \frac{EDV - ESV}{EDV} ]
where EDV = end-diastolic volume, ESV = end-systolic volume.
Experiment Results and Discussion
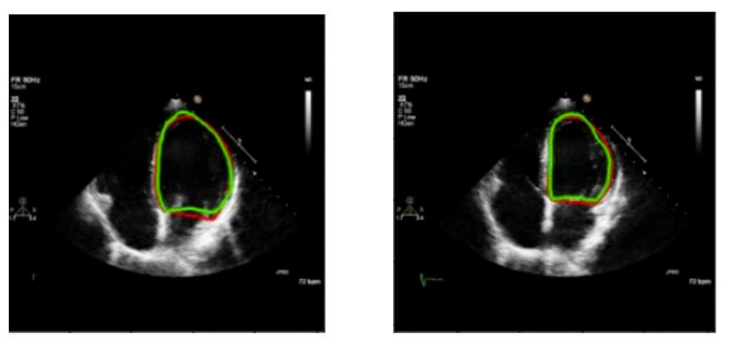
Fig. 3. End-diastolic (left) and end-systolic (right) images showing ground-truth (red) and predicted (green) borders.
Key Observations:
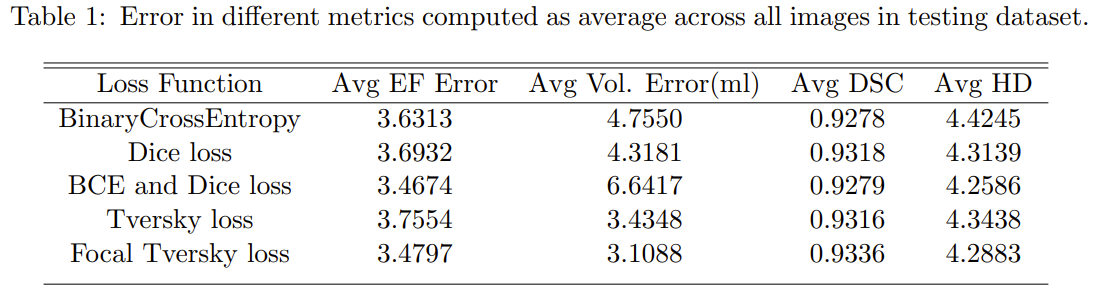
- Minimal variation in Dice coefficient (DSC) and Hausdorff distance (HD) across all loss functions
- Significant differences observed in Average Volume Error, showing that segmentation metrics alone are insufficient for evaluating cardiac performance
- BCE + Dice achieved high DSC but exhibited large volume errors
- Large volume errors can sometimes offset in EF computation, as seen in the example above (volume error = 17.6 ml, EF error = 2.38%)
These findings highlight that traditional metrics (DSC, HD) may not fully capture clinical accuracy when the goal is accurate EF estimation.
Future work focuses on assessing the generalizability of loss functions across different echocardiographic datasets to improve clinical applicability in LV function estimation.